What is Lymphoedema?
There are two types of lymphoedema Primary and Secondary. I was never informed of the type of lymphoedema I had, and I didn't realise I had secondary lymphoedema until I began running
L-W-O Community.
Lymphoedema is a chronic long-term disease that causes swelling in the body’s tissues. Lymphoedema patients mistakenly believe that it just affects their limbs, as do some medical professionals. However, it can also affect the breast, head, neck, or genitalia.
Many of us are unaware of the fact that our bodies include clusters of lymph nodes that are connected by a system of lymphatic vessels called the lymphatic system. White blood cells and antibodies are transported to your organs and tissues by the intricate network of ducts and capillaries that makes up your lymphatic system. Your immune system is strengthened by these cells and antibodies, which also aid in preventing infections.
To transfer the lymph through the veins, the lymph system must rely on muscle movements, and drinking water. Stress, exhaustion, inactivity, cold temperatures, infection, chemical or food additives, as well as age, can all slow down the body's normal lymphatic flow.
When the lymphatic system is unable to remove excess fluid, due to disrupted lymphatic pathways, swelling from fluid becomes uncomfortable and painful.
It is crucial that lymphoedema is identified and treated as soon as possible to prevent it getting worse and avoid damaging the lymphatic system further. Lymphoedema can be detrimental to both physical and mental health, and it is crucial to find support to improve your lymphatic health and wellbeing.
Chronic Oedema
The phrase "chronic oedema" refers to chronic illnesses that include the build-up of fluid and for which there is no known cure. The impact of chronic oedema on both the mental and physical wellbeing of a person’s life should not be underestimated.
Chronic oedema is classified as oedema that has been present for more than three months. It may coexist with lymphoedema but may be complicated by the following:
-
cardiac failure
-
immobility
-
venous disease
Immobility is likely to lead to oedema.
However, one of the known causes of lymphoedema is obesity. Fluid retention should not be ignored under any circumstances.
Controlling long-term illnesses can be enhanced if clinicians and patients come to an agreement on a care plan. However, it's crucial to understand that patients need to be motivated and given sound knowledge to support their own care.

Oedema is aggravated by:
-
standing or sitting in the same position for too long
-
eating too much salty food
-
being overweight
-
being pregnant
-
taking certain medicines – such as some blood pressure medicines, contraceptive pills, hormone therapy, antidepressants, or steroids
For further information on Oedema in ankles and legs visit this NHS information page.
Could I get lymphoedema if I haven't had lymph nodes removed?
Sadly
the answer is
yes
Unfortunately, there is no easy solution because there are two different types of lymphoedema, and additional causes can also cause lymphoedema. Furthermore, it is not clear why some people develop lymphoedema while others do not.
Below is a brief look at the types of lymphoedema with links for further reading.
Usually due to genetic underdevelopment or weakened lymph conducting channels, primary lymphoedema arises from a defect in the lymphatic system. Men, women, and children of any age can be impacted by this Read more...
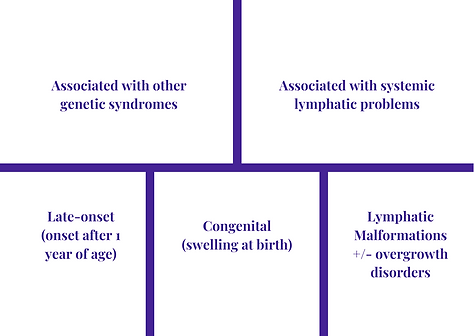
Above poster source: Dr. Kristiana Gordon, Lymphoedema Service, St. Georges, London, presented at BLS Conference 2018
Secondary Lymphoedema is a malfunction of a normally working lymphatic system that has been harmed by trauma, cancer treatment, obesity, or injury. Removal of lymph nodes, radiation, fungi, and cellulitis are also significant factors.
Immobility and being overweight may increase your risk of lymphoedema.
Early warning signs include swelling that does not go down overnight. Dry skin, skin folds, and thickening of the skin shouldn't be disregarded, and neither should pain, heavy limbs, clothing, or jewellery that leaves indentations or feels too tight.
Listen to what your body is telling you.
By applying pressure to the tissue, compression garments prevent fluid build-up and allow the fluid to drain.
Position yourself so that the lymph fluid can drain, whether you are sitting or lying down.
Your swelling will be reduced by elevating your limb position. Place your arm on a cushion or pillow if you have arm lymphoedema, make sure you are comfortable and not under any strain.
Your arm shouldn't extend past your shoulder. Avoid holding your arm in one posture for too long; ideally, change position every 30 minutes.
Lymphatic drainage techniques can remove a significant amount of congestion from affected areas.
Healthcare practitioners with the necessary training do manual lymphatic drainage (MLD).
Ask your healthcare provider to demonstrate basic self-lymphatic draining techniques for you to perform at home. Then, this will become a regular component of your self-care regimen.
Management and Treatment of Lymphoedema

I was initially given a list of dos and don'ts, the majority of which had no clear medical or scientific justification. L-W-O Community enjoys debunking myths; thus, we will do so whenever we can.
Your priorities are:
#GetMoving
#Hydration
Specialised massage - Manual Lymphatic Massage (MLD)
Self/Simple Lymphatic Drainage (SLD)
Don't allow your lymphedema to define who you are; do everything you can to overcome it. To prevent infection, take sensible precautions. Be kind to yourself and take care of your health. We are available to help. Join our support group.


Manual Lymphatic Drainage (MLD)
In the advanced therapy known as manual lymphatic drainage (MLD), the skin is moved in the direction of lymph flow using a variety of specialised, mild rhythmic pumping techniques.
This activates the lymphatic vessels, which transport elements crucial to the body's defence and remove waste.

Simple Lymphatic Drainage (SLD)
You include self/simple lymphatic drainage (SLD) in your self-care regimen.
Ask your nurse practitioner or therapist to demonstrate SLD so that you can do this at home. This massage takes about 20 minutes and is based on the more advanced MLD techniques.
To ensure regular lymphatic system stimulation, try to perform SLD at the same time each day. You can perform the massage with or without wearing your prescribed compression garments.
When you see your nurse practitioner/therapist for the first time your affected limb will be measured for compression hosiery which will help you maintain your swelling.
This works by putting pressure on the tissues to stop the build-up of fluid and helps the fluid drain from your affected limb.

Compression Pumps
Compression Pumps 'squeeze' a swollen limb in a sleeve or boot which inflates and deflates at regular intervals.
Lymph can be moved from the limb quite quickly, but it may collect in the trunk of the body causing discomfort.
Lymph may also return to the limb when the pump is removed. However, a pump may help to soften the tissues of the limb and for this reason your therapist would recommend usage.
Modern style compression pumps can mimic MLD.
Deep Oscillation
DOT is a patented electrostatic lymphatic massage therapy and clinically proven. The DOT Personal Unit is treatment that is delivered through light vinyl gloves or via special applicators when self-treating. This enables the user in self-management to reduce swelling, pain and can give a feeling of wellbeing.
The DOT can reduce pain, help with fibrosis, and scar tissue. The treatment is gentle, and the relaxing vibrations can penetrate to a depth of 8 cm this includes all tissue layers including the connective tissue.
Page first created September 2013
Last updated 01/09/2023
Next review September 2025





